Signs and symptoms of acute kidney failure may include:
Like proteinuria, a high creatine level is more an indication of a potential health problem, rather than a problem itself. If your creatine level increase is caused by a kidney issues, you may experience related symptoms. Kidney conditions often cause bladder and fluid retention issues. If your kidneys aren’t working well enough to remove toxins and waste from your body, you could notice a wide range of symptoms, including:
- Decreased urine output, although occasionally urine output remains normal
- Fluid retention, causing swelling in your legs, ankles or feet
- Shortness of breath
- Fatigue
- Confusion
- Nausea
- Weakness
- Irregular heartbeat
- Chest pain or pressure
- Seizures or coma in severe cases
Sometimes acute kidney failure causes no signs or symptoms and is detected through lab tests done for another reason.
When to see a doctor
See your doctor immediately or seek emergency care if you have signs or symptoms of acute kidney failure.
Causes
Acute kidney failure can occur when:
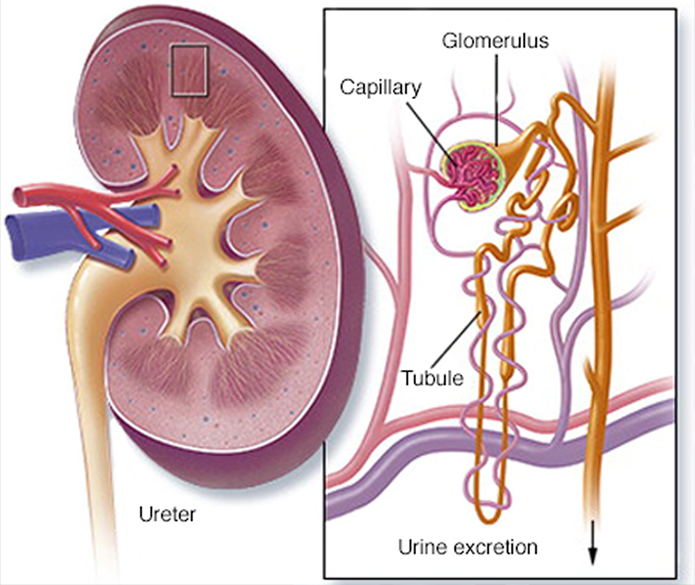
- You have a condition that slows blood flow to your kidneys
- You experience direct damage to your kidneys
- Your kidneys' urine drainage tubes (ureters) become blocked and wastes can't leave your body through your urine
Impaired blood flow to the kidneys
Diseases and conditions that may slow blood flow to the kidneys and lead to kidney injury include:
- Blood or fluid loss
- Blood pressure medications
- Heart attack
- Heart disease
- Infection
- Liver failure
- Use of aspirin, ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve, others) or related drugs
- Severe allergic reaction (anaphylaxis)
- Severe burns
- Severe dehydration
Damage to the kidneys
These diseases, conditions and agents may damage the kidneys and lead to acute kidney failure:
- Blood clots in the veins and arteries in and around the kidneys
- Cholesterol deposits that block blood flow in the kidneys
- Glomerulonephritis (gloe-mer-u-loe-nuh-FRY-tis), inflammation of the tiny filters in the kidneys (glomeruli)
- Hemolytic uremic syndrome, a condition that results from premature destruction of red blood cells
- Infection, such as with the virus that causes coronavirus disease 2019 (COVID-19)
- Lupus, an immune system disorder causing glomerulonephritis
- Medications, such as certain chemotherapy drugs, antibiotics and dyes used during imaging tests
- Scleroderma, a group of rare diseases affecting the skin and connective tissues
- Thrombotic thrombocytopenic purpura, a rare blood disorder
- Toxins, such as alcohol, heavy metals and cocaine
- Muscle tissue breakdown (rhabdomyolysis) that leads to kidney damage caused by toxins from muscle tissue destruction
- Breakdown of tumor cells (tumor lysis syndrome), which leads to the release of toxins that can cause kidney injury
Urine blockage in the kidneys
Diseases and conditions that block the passage of urine out of the body (urinary obstructions) and can lead to acute kidney injury include:
- Bladder cancer
- Blood clots in the urinary tract
- Cervical cancer
- Colon cancer
- Enlarged prostate
- Kidney stones
- Nerve damage involving the nerves that control the bladder
- Prostate cancer
Risk factors
Acute kidney failure almost always occurs in connection with another medical condition or event. Conditions that can increase your risk of acute kidney failure include:
- Being hospitalized, especially for a serious condition that requires intensive care
- Advanced age
- Blockages in the blood vessels in your arms or legs (peripheral artery disease)
- Diabetes
- High blood pressure
- Heart failure
- Kidney diseases
- Liver diseases
- Certain cancers and their treatments
Complications
Potential complications of acute kidney failure include:
Fluid buildup. Acute kidney failure may lead to a buildup of fluid in your lungs, which can cause shortness of breath.
Chest pain. If the lining that covers your heart (pericardium) becomes inflamed, you may experience chest pain.
Muscle weakness. When your body's fluids and electrolytes — your body's blood chemistry — are out of balance, muscle weakness can result.
Permanent kidney damage. Occasionally, acute kidney failure causes permanent loss of kidney function, or end-stage renal disease. People with end-stage renal disease require either permanent dialysis — a mechanical filtration process used to remove toxins and wastes from the body — or a kidney transplant to survive.
Death. Acute kidney failure can lead to loss of kidney function and, ultimately, death.
Prevention
Acute kidney failure is often difficult to predict or prevent. But you may reduce your risk by taking care of your kidneys. Try to:
Pay attention to labels when taking over-the-counter (OTC) pain medications. Follow the instructions for OTC pain medications, such as aspirin, acetaminophen (Tylenol, others), ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve, others). Taking too much of these medications may increase your risk of kidney injury. This is especially true if you have pre-existing kidney disease, diabetes or high blood pressure.
Work with your doctor to manage kidney and other chronic conditions. If you have kidney disease or another condition that increases your risk of acute kidney failure, such as diabetes or high blood pressure, stay on track with treatment goals and follow your doctor's recommendations to manage your condition.
Make a healthy lifestyle a priority. Be active; eat a sensible, balanced diet; and drink alcohol only in moderation — if at all
Diagnosis
If your signs and symptoms suggest that you have acute kidney failure, your doctor may recommend certain tests and procedures to verify your diagnosis. These may include:
Urine output measurements. Measuring how much you urinate in 24 hours may help your doctor determine the cause of your kidney failure.
Urine tests. Analyzing a sample of your urine (urinalysis) may reveal abnormalities that suggest kidney failure.
Blood tests. A sample of your blood may reveal rapidly rising levels of urea and creatinine — two substances used to measure kidney function.
Imaging tests. Imaging tests such as ultrasound and computerized tomography may be used to help your doctor see your kidneys.
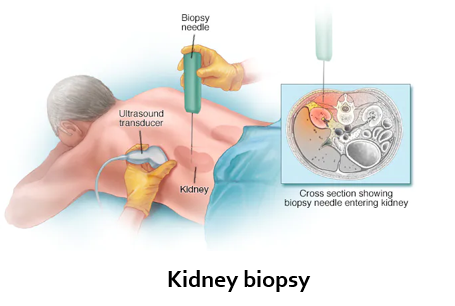
Removing a sample of kidney tissue for testing. In some situations, your doctor may recommend a kidney biopsy to remove a small sample of kidney tissue for lab testing. Your doctor inserts a needle through your skin and into your kidney to remove the sample.
Treatment
Treatment for acute kidney failure typically requires a hospital stay. Most people with acute kidney failure are already hospitalized. How long you'll stay in the hospital depends on the reason for your acute kidney failure and how quickly your kidneys recover. In some cases, you may be able to recover at home.
Treating the underlying cause of your kidney injury
Treatment for acute kidney failure involves identifying the illness or injury that originally damaged your kidneys. Your treatment options depend on what's causing your kidney failure.
Treating complications until your kidneys recover
Your doctor will also work to prevent complications and allow your kidneys time to heal. Treatments that help prevent complications include:
Treatments to balance the amount of fluids in your blood. If your acute kidney failure is caused by a lack of fluids in your blood, your doctor may recommend intravenous (IV) fluids. In other cases, acute kidney failure may cause you to have too much fluid, leading to swelling in your arms and legs. In these cases, your doctor may recommend medications (diuretics) to cause your body to expel extra fluids.
Medications to control blood potassium. If your kidneys aren't properly filtering potassium from your blood, your doctor may prescribe calcium, glucose or sodium polystyrene sulfonate (Kionex) to prevent the accumulation of high levels of potassium in your blood. Too much potassium in the blood can cause dangerous irregular heartbeats (arrhythmias) and muscle weakness.
Medications to restore blood calcium levels. If the levels of calcium in your blood drop too low, your doctor may recommend an infusion of calcium.
Dialysis to remove toxins from your blood. If toxins build up in your blood, you may need temporary hemodialysis — often referred to simply as dialysis — to help remove toxins and excess fluids from your body while your kidneys heal. Dialysis may also help remove excess potassium from your body. During dialysis, a machine pumps blood out of your body through an artificial kidney (dialyzer) that filters out waste. The blood is then returned to your body.
 Media Solutions
Media Solutions